Positioning Your Clients for 2026: Self-Funded Strategies for Brokers
As you prepare for another year of healthcare complexity and rising costs, one truth is clear: you cannot navigate this industry in a silo.
Client Expectations of a Partner
Employers expect you to bring forward partners – TPAs, PBMs, clinical vendors, stoploss, wellness solutions – that align to create an affordable, accessible, and personalized benefit to their members.
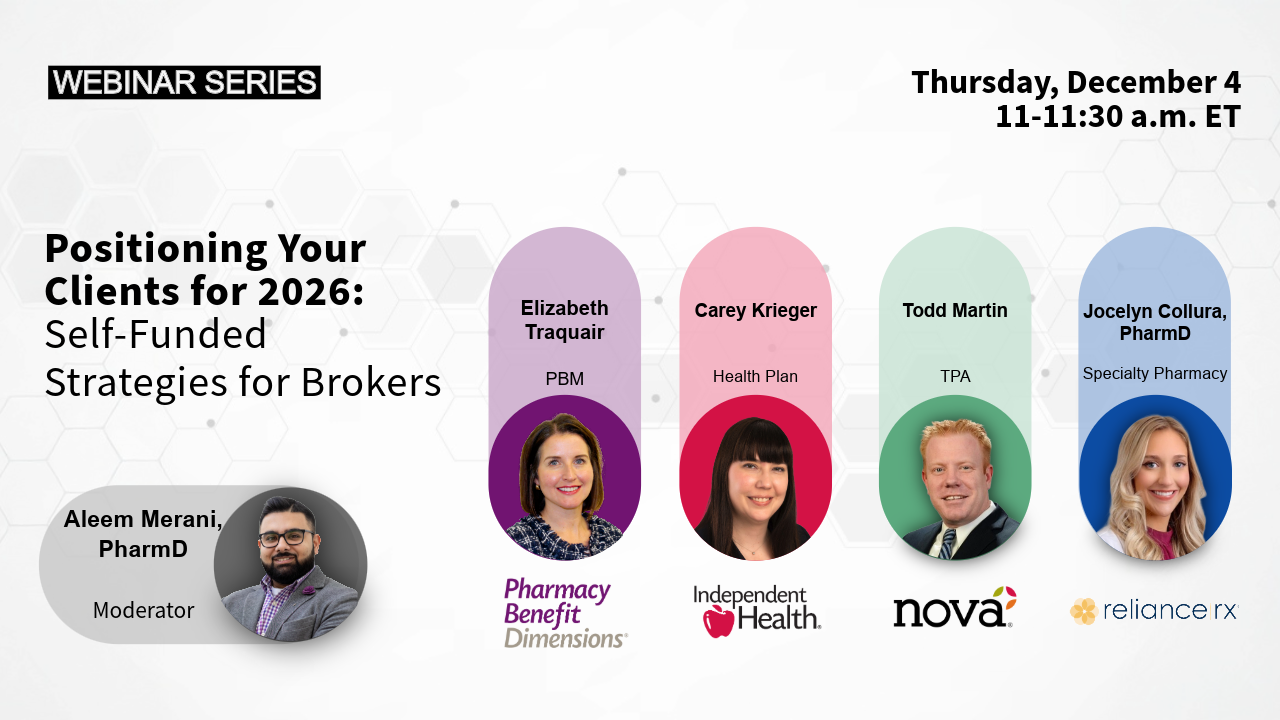
During our year-end webinar, “Positioning Your Clients for 2026: Self-Funded Strategies for Brokers,” PBDRx and a panel of healthcare experts highlighted opportunities brokers and consultants should leverage to protect budgets, elevate the member experience, and strengthen renewals in the year ahead.
Below is a recap of impactful, broker-focused insights including strategic questions you should be asking and actions you should be taking before renewals hit.
1. Leverage Self-Funding to Increase Control
Self-funded plans have risen in popularity as employers look for more control and customization in their healthcare strategy. Over two thirds of U.S. workers are covered by a self-funded health insurance plan, exhibiting a steady climb over the last two decades. Employer cost drivers include:
- Rising healthcare premiums that have outpaced inflation.
- Tighter company budgets and evolving workforce needs.
Technology Benefit: Telehealth
Self-funded plans are increasingly seeking innovative coverage options through virtual care to improve access, convenience, and cost efficiency. Employers who adopt integrated telemedicine services see ~43% savings to the health plan per visit. These services come with improved engagement and outcomes among members.
Broker Takeaways
- Identify clients who would benefit most from telehealth integration.
- If a telehealth program is presently offered, evaluate utilization as many brokers discover members aren’t using what’s already available.
- Quantify additional savings and develop member education strategies to improve benefit design and encourage members’ use.
Questions Brokers Should Ask
- Which clients will gain the most from virtual care steering based on claims?
- Is telehealth being communicated to the client and being utilized effectively?
2. Deliver Increased Predictability and Transparency with Level-Funded Plans
As costs rise and expanded solutions emerge, more small-to-medium sized employers are turning to level-funded models for:
- Budget stability
- Fully transparent claims data
- Customizable benefit design
Heading into 2026, adoption continues to accelerate because these plans offer predictability and control across a wide range of cost pressure, such as increased GLP-1 use and specialty medication pipeline volatility. The use of AI when evaluating eligibility and quoting will provide more opportunities for forecasting and lookback.
Broker Takeaways
- Review your book of business and identify clients who should evaluate level-funding as described above.
- Consider using AI to identify opportunities and risk when met with incomplete data.
Question Brokers Should Ask
- Which fully insured groups could benefit from a more predictable level-funded model?
3. Take Control of Specialty Costs with Strategic Clinical Integration
Specialty medications continue to dominate drug spend, despite less than 5% of the population requiring treatment with these drugs. Without proactive management, specialty costs will continue to impact renewals and new opportunities.
Partners with strong specialty programs, proactive care management, and site-of-care optimization can reduce costs by up to 60% while significantly improving adherence and outcomes.
Upcoming 2026 biosimilar and generic launches for Xolair, Simponi, Perjeta, and Orencia* will create major savings opportunities for self-funded employers who are willing to adopt smart clinical programs.
It’s also important to note that significant reimbursement differences persist between outpatient hospitals and alternative sites of care. There is a potential savings of 30-60% for employers who work with a specialty pharmacy to take advantage of Site-of-Care (SOC) management opportunities.
Broker Takeaways
- Request a specialty disruption forecast for your top 510 cost drivers.
- Evaluate your PBM partner’s hands-on approach to managing biosimilar conversion.
- Review site-of-care data for medications billed under the wrong benefit and work with your client to educate members about resources available in their area.
Questions Brokers Should Ask
- Am I confident that my partners can guide cost-effective utilization as biosimilars launch?
- What specialty categories are trending upward in my book – and do I know why?
4. Prepare Clients for 2026 Medicare Changes and IRA-Driven Drug Changes
The Inflation Reduction Act and the Medicare Drug Price Negotiation Program will reshape pricing for these 10 drugs:
- Eliquis
- Jardiance
- Xarelto
- Januvia
- Farxiga
- Entresto
- Enbrel
- Imbruvica
- Stelara
- Insulin-aspart products (Fiasp, Novlog, etc.)
These changes will influence benefit design, cost, and member experience. Brokers who help clients anticipate these changes – not just react to them – will be in the best position to guide strategy in a shifting regulatory landscape.
Broker Takeaways
- Educate clients early on IRA changes and shifting price dynamics.
- Coordinate with PBM to get a sense of change of plan and risk.
Questions Brokers Should Ask
- How exposed are my clients to drugs affected by IRA price negotiation?
- Do I have a communication plan to inform employers of changes?
Turn Insight into Strategy for 2026
Healthcare is becoming more complex, more regulated, and more costly, but also more integrated. With a focus on managing risk and cost, clients increasingly seek to work with consultants and brokers who understand their needs and make data-informed decisions in alignment with the right healthcare partners,
At PBDRx, we and our partners are here to help brokers turn strategic insights into actionable, client-focused solutions.
Want to dive deeper into how these trends apply to your book of business? Let’s schedule a new year strategy session to start the new year with clarity, control, and confidence.
*Note, not all listed medications will be added to plan formularies.

